Fueling Focus in Childhood ADHD
How nutrition, sleep, and daily habits can help your child thrive
If you frequently find yourself dropping off forgotten lunches or snacks, or reminding your child for the tenth time to put on their shoes, you already know: parenting a child with ADHD can feel like a full-contact sport. Between juggling school demands, after-school activities, and emotional ups and downs, mealtimes often become another source of stress.
Here’s the encouraging truth – while ADHD can’t be “fixed” through food, nutrition and lifestyle are powerful tools that can make everyday life calmer, more focused, and more manageable. When we nourish the body and brain consistently, we support better attention, steadier moods, and more predictable energy.

Understanding ADHD – and Why Nutrition Matters
ADHD (Attention-Deficit/Hyperactivity Disorder) is a neurodevelopmental condition tied to differences in how the brain regulates focus, motivation, and impulse control. It involves chemical messengers, mainly dopamine and norepinephrine, that don’t always work as efficiently. Genetics play a big role, but so do environmental and lifestyle factors. We know that prenatal exposures, prematurity, or environmental factors like lead can play a role. None of this is about fault; it’s about understanding the “why” so we can target the “what now.”
Because every child with ADHD is unique, the best approach is multifaceted and collaborative. Pediatricians, psychologists, educators, and increasingly, registered dietitians, all contribute pieces of the puzzle. Nutrition can’t replace medication or behavioral therapy, but it can make those strategies work better, giving the brain the raw materials and rhythm it needs.
The Sleep-Focus Connection
Sleep difficulties are extremely common in ADHD, and they often form a frustrating loop: poor sleep worsens focus, and ADHD symptoms make it harder to fall or stay asleep.
Nutrition can quietly support sleep quality:
- Evening meals that include complex carbs (like brown rice, sweet potatoes, or quinoa) help the brain make serotonin and melatonin.
- Magnesium-rich foods – leafy greens, pumpkin seeds, and almonds – promote relaxation.
- Avoiding caffeine and large amounts of added sugar after 2 p.m. can prevent bedtime restlessness.
Good sleep hygiene is equally vital: consistent bed/wake times, dark rooms, no screens an hour before bed, and regular outdoor play all help regulate circadian rhythm, the body’s internal clock that governs focus by day and rest by night.

The Gut-Brain-ADHD Connection
Science is catching up with what many parents notice intuitively: when digestion is off, attention and behavior often follow.
The gut is home to trillions of microbes that send constant messages to the brain via the gut–brain axis. These microbes influence inflammation, mood, and even the production of neurotransmitters like serotonin and dopamine.
Supporting the gut starts with simple, real-food habits:
- Include fiber-rich foods (fruits, veggies, beans, oats) daily. Fiber feeds beneficial bacteria.
- Add fermented foods like yogurt, kefir, sauerkraut, or miso to diversify gut microbes.
- Minimize ultra-processed foods and dyes, which can disrupt gut balance and blood sugar regulation.
A healthy gut can’t “cure” ADHD, but it lays a solid foundation for better focus, calmer moods, and more stable energy.
Dietary Patterns That Support Focus
Children with ADHD benefit from a steady, balanced approach to meals and snacks, emphasizing real foods and stable blood sugar. When glucose swings high and low, attention and mood swing right along with it.
Aim for:
- A mix of protein + fiber + healthy fat at every meal.
- Predictable meal and snack times: consistency helps regulate appetite and energy.
- Hydration! Even mild dehydration can reduce concentration.
Example ADHD-friendly day:
- Breakfast: Oatmeal topped with berries, chia seeds, and almond butter.
- Lunch: Turkey and cheese on whole-grain bread, carrots + hummus, apple slices.
- Snack: Greek yogurt with fruit or a handful of nuts.
- Dinner: Baked chicken or tofu, brown rice, roasted vegetables.
Compare that to the classic “grab-and-go” pattern, like sugary cereals, skipped breakfasts, or processed snacks, which tends to cause energy crashes and afternoon meltdowns.

Key Nutrients Linked to ADHD Support
Certain nutrients play especially important roles in brain function. Here’s what the research, and our experience in practice, tells us:
Omega-3 Fatty Acids
EPA and DHA (found in salmon, tuna, sardines, walnuts, chia, and flax) are essential for brain structure and signaling. Studies suggest omega-3s can modestly improve inattention and emotional regulation in some children. For picky eaters or kids who rarely eat fish, a high-quality supplement may be helpful, but always confirm dosage with your healthcare provider.
Iron & Zinc
Both support dopamine activity. Low iron or zinc has been associated with more severe symptoms and poorer treatment outcomes. Foods like lean red meat, lentils, beans, nuts, and fortified cereals can help meet needs. Because excess iron isn’t harmless, test before supplementing.
Vitamin D
Beyond bone health, vitamin D influences mood and brain development. Deficiency is common, especially in northern climates. Good sources: sunlight, fortified milk or plant milks, and fatty fish. Ask your child’s provider about testing.
Magnesium & B Vitamins
Magnesium calms the nervous system and supports sleep; B6 and B12 aid neurotransmitter synthesis. Think leafy greens, seeds, eggs, poultry, dairy, and whole grains.
Probiotics
Emerging studies show certain probiotic strains may improve quality of life and behavior, likely by balancing gut bacteria and reducing inflammation. Rather than self-supplementing, start with probiotic foods and review options with your dietitian.
Copper & Lead
Excess copper relative to zinc, and any lead exposure, can negatively affect attention and cognition. If your home was built before 1978 or you have concerns about plumbing or environmental exposure, talk to your pediatrician about testing.
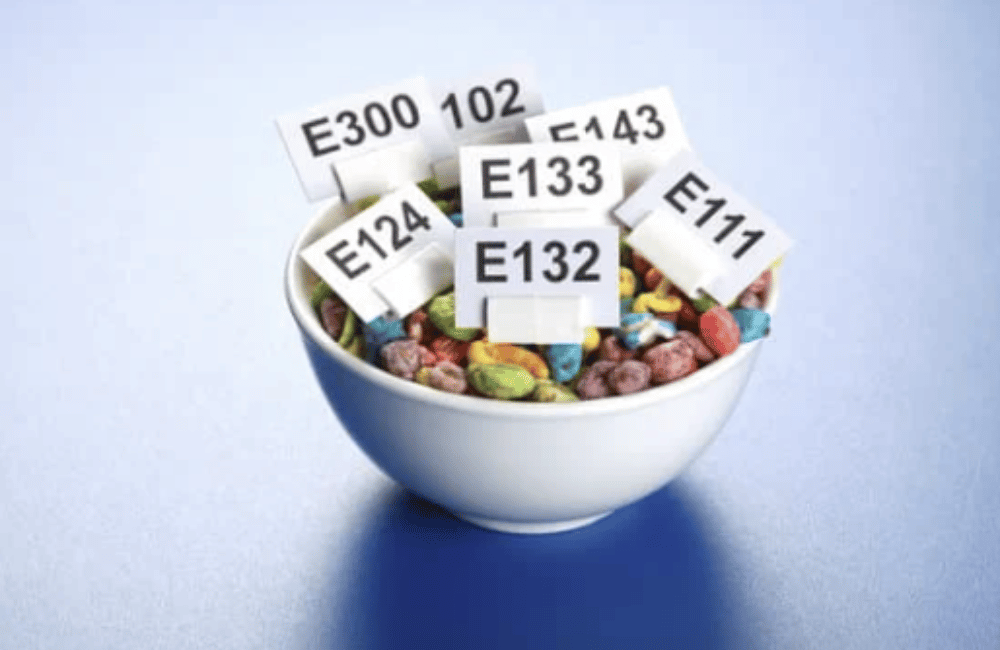
What About Food Additives?
Artificial colors (like Red 40 and Yellow 5), preservatives (sodium benzoate, BHA, BHT, TBHQ), and flavor enhancers have long been suspected of worsening hyperactivity in sensitive kids. Research shows some children are indeed more reactive, while others are unaffected.
Since dyes and preservatives add no nutritional value, many families simply choose to avoid them. Start small: swap brightly colored drinks and snacks for whole-food options, and note any changes in attention or mood.
Elimination Diets – Proceed with Care
Some studies show that strict elimination diets can reduce symptoms in a subset of children, but these should never be attempted without professional guidance. Removing entire food groups can quickly cause nutrient deficiencies and growth issues.
If a trial is warranted, a dietitian can design a short-term plan with careful tracking and safe re-introductions. The goal isn’t restriction, it’s clarity. A well-planned, supervised elimination of foods can help identify food triggers.
Practical Strategies for Busy Families
Managing ADHD nutrition doesn’t have to be complicated. Consistency and environment matter just as much as the food itself.
A Few Core Habits
- Keep a rhythm: three meals + two snacks, around the same times each day.
- Front-load protein: breakfast with eggs, yogurt, or smoothies with protein sets the tone for focus.
- Batch prep on calm days: wash produce, portion snacks, or freeze mini muffins for grab-and-go options.
- Make the healthy choice visible: keep fruit at eye level and water bottles filled.
- Limit chaos at meals: turn off screens, sit together when possible, and make eating a relaxed moment instead of a battleground.
Quick Wins This Week
- Add one extra fruit or veggie per day – smoothies and veggie muffins count.
- Offer protein at every meal, even if it’s just nut butter or cheese.
- Swap one packaged snack for a whole-food version.
- Get outside together after school. Movement helps regulate both focus and sleep.
- Model mindful eating: pause, breathe, and enjoy your own plate too.
When to Loop in a Registered Dietitian
A pediatric dietitian can:
- Evaluate nutrient gaps and growth trends.
- Build realistic meal plans for picky eaters.
- Help identify possible food sensitivities safely.
- Recommend targeted supplements when appropriate.
- Coordinate with your pediatrician, OT, or speech-language pathologist if feeding mechanics (biting, chewing, swallowing) are a concern.
Dietitians are translators, turning complex science into practical steps that fit real family life.

Moving Forward
ADHD management works best when we treat the whole child, not just the symptoms. Balanced meals, consistent routines, outdoor play, and adequate sleep all shape how a child feels and functions day to day.
When families build these foundations, medications (if used) work more effectively, school days feel smoother, and kids start to feel more confident in their own bodies.
If your child struggles with attention, hyperactivity, or mealtime battles, you don’t have to navigate it alone. Nutrition can be a meaningful piece of the plan, one we can personalize to your child’s unique needs and preferences.
FAQ: Nutrition & ADHD
Is there a specific “ADHD diet”?
There’s no one-size-fits-all plan. Most children benefit from balanced, protein-rich meals, steady blood sugar, and minimizing processed foods and dyes. We individualize it for each child’s needs.
Do we need to remove gluten or dairy?
Only if there’s a known intolerance or clear symptom link. For most kids, eliminating whole food groups isn’t necessary, and we always trial such changes carefully under professional guidance.
Should my child take supplements?
Sometimes! Nutrients like omega-3s, iron, zinc, and vitamin D can support brain health, but testing and dosing should always be supervised. Food first, supplement when needed.
Can nutrition replace ADHD medication?
No, but it can make other treatments work better. Nutrition supports brain chemistry, energy, and focus so your child feels and functions their best.
Ready to take the next step?
We love helping families uncover simple, sustainable nutrition strategies that support attention, growth, and calm energy.
Book a pediatric nutrition consult today to start building a plan that works for your child and your family.
Medical Disclaimer:
The information provided on this blog is for educational and informational purposes only and is not intended as a substitute for medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider, such as your physician, pediatrician, or a registered dietitian, before making any changes to your or your child’s diet, health routine, or treatment plan.
While we are a medical practice specializing in integrative and functional nutrition, the content shared here reflects general knowledge and holistic guidance, and may not be appropriate for every individual. Reliance on any information provided on this site is solely at your own risk.
References
(Kept concise for readability; full citations available upon request)
NIMH. ADHD Overview, 2024 • AAP. ADHD Patient Care, 2022 • Becker SP et al., Curr Opin Psychol 2020 • Heilskov Rytter MJ et al., Nord J Psychiatry 2015 • Sibley MH et al., Lancet Child Adolesc Health 2023 • Granero R et al., Nutrients 2021 • Khoshbakht Y et al., Eur J Nutr 2021 • D’Helft J et al., Nutrients 2022 • Lukovac T et al., Children (Basel) 2024 • Lange KW et al., Curr Nutr Rep 2023 • Robberecht H et al., Molecules 2020


