Female Fertility Diet and Lifestyle
Diet and Lifestyle Considerations for Fertility
If you are considering starting a family, expanding your family, struggling with infertility, or have experienced failed pregnancies, there is no shortage of rabbit holes to explore in terms of the best diet, supplements, and lifestyle factors to improve your chances of success. No matter your current circumstances, you have control over many daily choices that affect reproductive health.
Our bodies are complex systems. There are many factors involved in pregnancy and infertility. We know that lifestyle factors including nutrition and diet, toxin exposure, stress management, exercise, and body weight affect fertility.
This post will provide education on potential causes of female infertility, oxidative stress and how it impacts fertility, and diet and nutrition to promote fertility. Throughout, the terms female, woman, and women are referring to people who were assigned female at birth (AFAB).

Conception
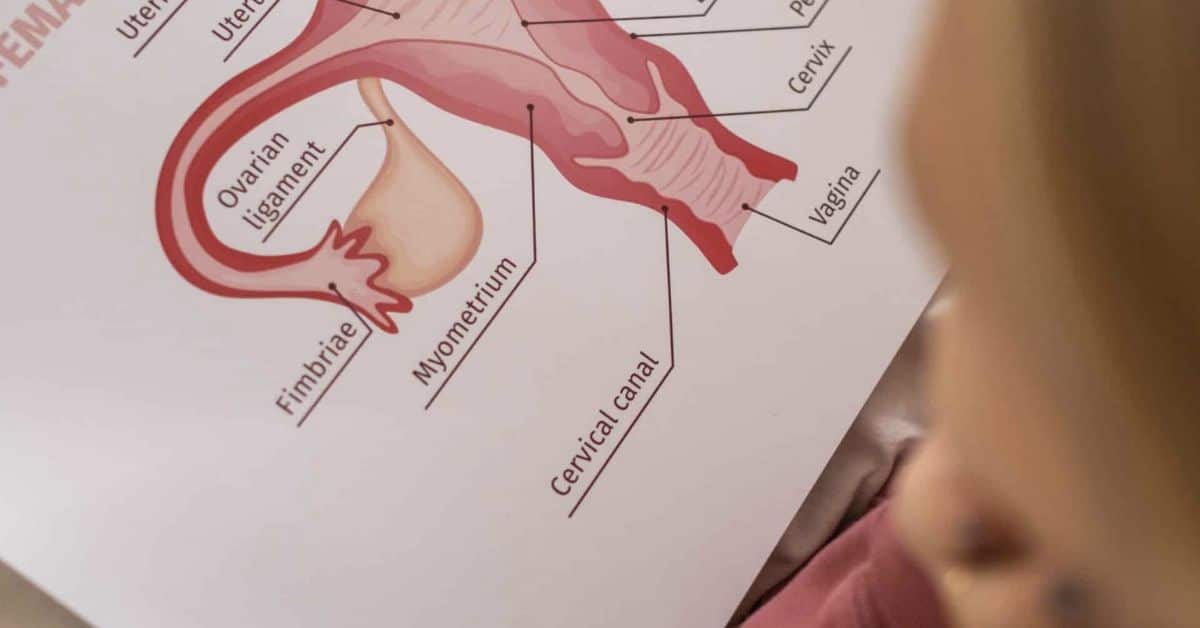
Briefly, we will review conception, as there are numerous steps to this process that need to be perfectly synchronized to result in pregnancy. Ovulation is one of four phases in the menstrual cycle. After a mature egg is released from an ovary, sperm must join the egg and fertilize it, creating a zygote. The fertilized egg travels through the fallopian tube to the uterus and attaches to the inside uterine wall. This is called implantation. In a successful pregnancy, the fertilized egg becomes an embryo. Over months, the embryo develops into a baby.
There are billions of chemical and physical transactions that need to take place for the zygote to develop into a healthy fetus, achieving the ultimate goal of having a baby. Taking care of the body’s reproductive system gives us the best chance to conceive.
What is Infertility?
Infertility is when a couple has been trying to get pregnant using planned timing (having sex when the woman is ovulating, determined using ovulation strips if needed), or having unprotected sex for at least one year without successful pregnancy. It is recommended that women over the age of 35 seek medical support if they do not become pregnant within six months of trying (versus 12 months if under the age of 35).
Recurrent (two or more) pregnancy losses or miscarriages are also considered when diagnosing infertility. Conception is typically lost during implantation. Many pregnancies fail for unknown reason after the pregnancy has been verified by a pregnancy test. It is estimated that 30-50% of pregnancies end spontaneously in the first trimester. As many as 15-20% of clinical pregnancies (meaning the doctor has verified through ultrasound that there is a gestational sac, yolk sac, fetal pole and fetal heartbeat), end in spontaneous abortion. This is why many women choose to wait until 12 weeks to share their good news with friends and family.
When a pregnancy fails, it does not mean that the woman did something wrong. It is important to know that it is very common and that there are support groups and resources that can help process the emotional rollercoaster that comes with trying to become pregnant. Chances are that most women have a friend, acquaintance, or family member who can relate to what they are experiencing. Our bodies are intelligent, and most of the time it will not allow a pregnancy to continue unless the zygote is healthy.
According to the American Society for Reproductive Medicine, one in seven couples, or 14%, experience infertility. It is estimated that one third of these cases are caused by female factors, roughly the same amount of couple factors, and 20% from male factors. If you think you might be experiencing infertility, the first step is to seek help by discussing your concerns with your primary physician or obstetrician gynecologist.

Female Infertility Causes
Female infertility causes are due to a number of conditions. We will just touch briefly on them. Talk to your doctor if you’re concerned that any of these conditions may be causing infertility.
- Anovulation – affects roughly 25% of infertility cases, where the woman’s ovaries are not producing and/or releasing eggs at regular rates during menstruation. This can be caused by a variety of factors.
- Female aging and diminished ovarian reserve – more people are choosing to have children later in life. As females get older their number of eggs and quality of eggs lessen, decreasing chances of conception.
- Fibroids or polyps – non-cancerous tumors that develop in the uterus and can affect the ability of the uterus to implant an egg. This is one of the most common uterine issues that may cause infertility.
- Polycystic Ovary Syndrome (PCOS) – an endocrine disorder that weakens fertility by causing a woman’s eggs to fail before growing into an embryo. Approximately 10% of women in the United States have PCOS during child bearing age.
- Pelvic Inflammatory Disease (PID) – results from a sexually transmitted disease or infection that can lead to damaged and scarred fallopian tubes, ovaries and uterus.
- Tubal factor infertility – when the woman’s fallopian tubes prevent sperm from reaching the egg to fertilize it or preventing the fertilized egg from reaching the uterus for implantation.
- Ectopic pregnancy – this occurs when a fertilized egg attaches itself outside the uterus, usually in the fallopian tubes and requires medical intervention.
- Endometriosis – when the tissue of the uterus, referred to as the endometrium, grows on the outside of the uterus rather than in it.
- Unexplained infertility – affects roughly 10% of couples, but this isn’t determined until both male and female, if applicable, have been tested for infertility.
- Hormonal imbalances – can be caused by a number of different reasons, environmental, genetic and physical. Some signs of this may be a missing menstrual cycle (amenorrhea), irregular or inconsistent menstrual cycles, referred to as oligomenorrhea and characterized by fewer than eight periods a year, cycles lasting longer than 35 days, or shorter than 21 days, or painful, heavy menstrual cycles (menorrhagia).
- Body Mass Index (BMI) – a BMI that is very high or very low may decrease your chances of getting pregnant due to altering hormone levels and ovulation.
- Intense, frequent sport – competitive athletes or women who exercise intensely and frequently could be at risk for something called Relative Energy Deficiency (REDS). This energy deficiency can stem from undereating, either purposefully or unintentionally, as a result of too intense exercise or poor eating habits. Some examples are cross country running, aesthetics sports like gymnastics or ballet, swimming, and cross country running. When trying to conceive it may be beneficial to cut back on intensity in exercise. It is recommended that adults get at least 30 minutes of moderate intensity exercise each day. If overweight and trying to lose weight to conceive, intense exercise and HIIT style workouts may help to acheive goals faster. Intense exercise is associated with taking longer to conceive for normal weight women. This is why vigorous exercisers are cautioned to cut back exercise to a moderate amount when trying to conceive. Contact sports like football, rugby, hockey, volleyball and kickboxing should be avoided avoid hard impact and hitting the abdomen.
Your medical team can help determine if there are underlying conditions that are causing infertility. Sometimes, there is nothing you can do from a nutritional standpoint to increase fertility. However, improving your diet can help increase fertility with some conditions.
One thing is certain – everyone benefits in a multitude of ways by adopting a healthy diet.

Oxidative Stress
Oxidative stress (OS) occurs when there are not enough antioxidants (helpful molecules that repair damage to cells) available to combat reactive oxygen species (ROS, also known as free radicals). ROS are part of normal metabolism but left unchecked cause harm and death to our cells. ROS cause a chain reaction of damage throughout the body. This chain reaction is associated with chronic disease and negatively affects fertility.
The most modifiable risk factors that contribute to OS are diet and exercise. A poor diet high in processed and inflammatory foods and lacking in healthful plant foods and lack of exercise cause OS. Other factors that can often be addressed with lifestyle changes are chronic excess stress and exposure to chemicals and toxins. Oxidative stress may cause damage to oocytes, that is, immature female eggs in the ovaries. This leads to defective fertilization. If fertilization is still achieved, oxidative stress can still result in embryo fragmentation, which decreases the risk of successful pregnancy; implantation failure, where the fertilized egg will not be able to implant into the uterus walls, and therefore, the pregnancy is not able to continue; placenta development could be damaged; and congenital abnormalities may result. Oxidative stress may also create insufficient luteinizing hormone (LH), which is responsible for continuation of pregnancy.
There are many ways that OS can negatively impact fertility. It makes sense to try to reduce OS. One way to do that is through balancing ROS with antioxidants, which can be incorporated naturally into the diet. In some cases, supplements may also help support the body’s natural antioxidant system. Getting adequate exercise, adopting stress management techniques, incorporating mindfulness practices, and limiting toxin exposure are also ways to reduce oxidative stress.

Toxins and Fertility
In recent years, widespread interest in the effects of toxins on fertility has grown. Increasingly, research tells us that there is an association between environmental toxin exposure and infertility. Toxins in our environment contribute to overproduction of ROS, cell damage, cell death, DNA damage, and interfere with signaling pathways involved in cell growth, cell division, organ growth, formation and development of embryos, and changes in gene expression necessary to grow a healthy baby.
In our practice, we recognize that discussing toxin exposure concerns many of our clients, as it is difficult to avoid them. It would be virtually impossible in the modern world to eliminate your exposure to environmental toxins. The good news is that it is okay to start with small, simple steps to reduce toxin exposure, and to grow from there. Trying to conceive is enough of a stressor for most people we work with. We certainly do not want to add to that stress by overfocusing on things that are not within our control. Some of the toxins that we advise our clients to avoid, because there is evidence they may affect fertility, are bisphenol A (BPA), phthalates, lead, arsenic, mercury, persistent enviromental pollutants (POPs) like glyphosate and dioxin, glycol ethers (DEGME and EGBE) organic solvents, pesticides used on produce like atrazine, and perflourinated chemicals (PFAS). Whew. Seems daunting, right?
We help our clients create a plan to reduce toxin exposure by focusing on the low-hanging fruit first. Some tips we may offer include:
- Start to replace skincare products (makeup, lotions, soaps) with natural alternatives as you run out
- Replace household cleaners with natural alternatives as you run out
- Replace plastic containers with ceramic and glass
- Never microwave plastic containers, and hand wash plastics
- If you paint your nails or color your hair, wear a mask
- Avoid handling paper receipts – always choose the email receipt when that is an option
- Purchase organic produce as often as possible. This is less important with thick-skinned produce that the peel is removed from
- Buy wild caught fish and organic meat, poultry, dairy, and soy
- Avoid canned foods when you can, and look for BPA-free on can labels
This is a short list, but mostly simple things anyone can start to do. If this is a new concept for you, choose one to two items at a time to get started. We also encourage our clients to check out other resources. A few helpful websites we regularly recommend are www.ewg.org, toxicfreefuture.org, and www.itstartswiththeegg.com.
Supplements and Nutrients to Improve Fertility
Nutrients
When trying to conceive, it is ideal to consider diet and lifestyle and start making changes at least three months prior to trying to conceive. This includes taking a prenatal vitamin. A prenatal vitamin supplements nutrients needed to grow a healthy baby. Folate is essential in pre-pregnancy to decrease the risk of neural tube defects. Vitamin B12 helps prevent spina bifida and other spinal and nervous system birth defects. It is recommended to get at least 600 mcg/day of folate and 2.6 mcg/day of B12 when trying to conceive. Vitamin D also plays a role in female fertility. The recommended dietary allowance (RDA) for pregnant and breastfeeding women is 600 IU or 15 mcg vitamin D.
It may benefit some women to check nutrient levels, such as iron and vitamin D. Iron needs increase from 18 mg/d to 27 mg/d during pregnancy. Many women are low in iron at baseline, and pregnancy is a leading cause of iron deficiency anemia. We do not recommend taking iron supplements without getting iron labs done and/or speaking with a healthcare professional, as too much iron is toxic for the body. Women living in nothern climates, who are overweight, or have dark skin, should have vitamin D levels checked, as all three of those reasons increase risk of vitamin D deficiency, which can negatively affect fertility. If vitamin D is low, most prenatal vitamins do not contain sufficient vitamin D to make improvements.
Other micronutrients with increased needs during pregnancy include vitamin A, vitamin C, thiamin, riboflavin, niacin, vitamin B6, pantothenic acid, choline, chromium, copper, iodine, magnesium, manganese, molybdenum, selenium, and zinc. Prenatal multivitamins typically have greater than the RDA of most micronutrients. A prenatal vitamin in addition to a well-planned diet is adequate supplementation for most women trying to conceive. Women with special dietary needs or certain health conditions may need to pay closer attention to their diets. For example, vegan diets tend to be lower in choline than omnivore diets. A registered dietitian can provide guidance on food and supplements, and is a beneficial addition to the prenatal support team.
Antioxidant Supplements
Supplementing with antioxidants could be beneficial due to their ability to help combat oxidative stress (OS). Recall that OS is an imbalance of antioxidants and free radicals. As discussed, free radicals are uncharged molecules in the body that can cause chain-reaction damage to various systems, including reproductive health. Antioxidants that combat free radicals and may improve egg quality and fertility include glutathione, alpha-lipoic acid (ALA), vitamin E, vitamin C and ubiquinone/coenzyme Q10 (CoQ10).
Glutathione is a naturally occurring detoxifier of excess reactive oxygen species. ALA can quench free radicals and scavenge ROS. Vitamin E and vitamin C work together to repair damage to cells caused by ROS. CoQ10 is a molecule that our bodies make and is in every one of our cell membranes. CoQ10 helps our bodies to increase production of antioxidants and reduce OS. There is evidence that CoQ10 is beneficial for fertility. An elevated level of reactive oxygen species (ROS) is seen in those with unexplained infertility, as well as PCOS and endometriosis, and therefore could be a major contributor to infertility in males and females. However, glutathione has not been studied thoroughly enough to improve natural fertility directly. Lipoic acid has been shown to lower several inflammatory markers and help improve the balance between OS and depleted antioxidants.
Start taking a prenatal multivitamin one to three months prior to trying to conceive to ensure your body isn’t deficient in essential nutrients needed for pregnancy. Consider taking an antioxidant supplement like CoQ10 to combat oxidative stress in the body, which has been linked to infertility.
A dietitian can review the current diet and help determine what nutrients may be lacking. Consult with a dietitian or other healthcare provider knowledgeable in supplements prior to beginning any supplement regimen. Healthcare providers who are well versed in supplements know that not all supplements are created equal and will provide specific recommendations on formulations, brands, and dosages. Like everything else, some are higher quality than others. High quality supplements are batch tested, have less fillers, and more bioavailable ingredients. Supplements are meant to complement the diet, and what is beneficial for one person may not be helpful for someone else.

Women with PCOS
Women with PCOS typically have impaired insulin function, higher rates of depression and anxiety, and are more likely to have higher BMI. Research suggests that supplementation of myo-inositol and d-chiro-inositol could be beneficial for PCOS women trying to conceive, as they are found to be deficient in inositol and have dysregulated insulin levels. Supplementation in a ratio of 40(myo-inositol):1(d-chiro-inositol) helps restore hormonal and metabolic parameters like blood lipids (fats), insulin sensitivity and systolic blood pressure, which can be skewed in patients with PCOS. It can also help improve egg quality, ovulation, insulin and inflammation in the body. Ovasitol is an over-the-counter supplement made in a 40:1 ratio, like that naturally occurring in the body, but it is suggested that your doctor prescribe you the right ratio and supplementation.
Omega-3 fatty acids, like those found in fatty cold water fish and some nuts and seeds, are the building blocks of cell membranes and hormones. It is recommended that everyone eat eight ounces of fish per week, or four ounces two times per week, according to the Dietary Guidelines for Americans. However, most people are not doing so. Therefore, it might be beneficial to supplement with fish oil, which has both eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). There are algae oil products for people who avoid animal products or have allergies.
One study found that 6 months of supplementation with omega-3 fatty acids increased white cells and good cholesterol profile, decreased bad cholesterol profiles and blood triglycerides (fats), decreased testosterone, improved menstrual cycle regularity, and decreased inflammation in the body. However, there was not a significant change in weight, number or size of ovarian follicles (potential eggs), or menstrual bleeding. This supplementation would be beneficial with other healthy lifestyle changes. It is also worth noting that omega-3 fatty acid supplementation has been found to improve mood, and since PCOS sufferers are more likely to have anxiety, depression, insulin resistance and inflammation in the body, supplementation is worth considering to help alleviate these symptoms.

Foods that Promote Fertility
Beneficial Foods
Healthy, anti-inflammatory dietary patterns, such as the Mediterranean diet or the “Fertility Diet Pattern” have been seen to have positive effects on fertility. These diets are rich in whole food sources of healthy fats, grains, fruits, veggies, beans and lentils, nuts and seeds, and herbs and spices. About two servings of fatty fish are recommended each week. Anti-inflammatory diets limit or omit red and processed meats, and include moderate amounts of cheeses and wine. Most flour based grain foods and packaged foods and snacks would not be recommended. A “Fertility Diet Pattern” was created by Harvard Education in a 2007 study and has been found to positively affect chances of conception.
These types of dietary patterns are rich in antioxidants found in fruits and vegetables, essential vitamins like vitamin C, vitamin A, vitamin E, B vitamins like thiamin, riboflavin, folate, and niacin, and minerals like magnesium, potassium, calcium, iron and zinc. All of these play some role in the process of becoming pregnant and combating oxidative stress.
Fertility Diet Protocol
- Include monounsaturated fats like olive oil and avocados, nuts, almonds, cashews, peanuts, and olives
- Eat more vegetarian protein and iron sources like soy, lentils, nuts, and beans
- Include full fat dairy foods, and limit low fat or skim milk options for yogurt and cheeses
- Eat more high fiber, low glycemic carbohydrates like whole grains, whole fruits, and whole vegetables
- Eat moderate amounts of animal foods from sources like dairy, eggs, and poultry
- Avoid trans and saturated fats found in red and processed meat and processed foods like chips, cookies, crackers, butter, fried foods
- Limit processed, refined carbohydrates like white bread, white pasta, white rice, cookies, cakes, and baked goods
Foods to Limit or Avoid
Foods that have been linked to have negative effects, meaning higher rate of infertility, are: high intake of saturated and trans fat, red and processed meats, potatoes, sweets, sugar sweetened beverages like energy drinks and soda, high intakes of fast food, and an absence of regular consumption of seafood like salmon and shrimp.
Other Considerations
Foods that have not been found to have an effect on female fertility are: caffeine, soy, vitamin D, dairy products, alcohol, diet soda and fruit juice. While caffeine consumption has no known effects on fertility, it is correlated to some potential effects in pregnancy and has been linked to a potential increased risk of miscarriage, stillbirths, low birth weight or small for gestational size, preterm birth, childhood acute leukemia, childhood overweight, and obesity later in life. Therefore if you’re trying to conceive, it may be beneficial to cut caffeine early on.
We do not condone alcohol use by women who are trying to conceive or who are pregnant, as alcohol is a toxin and can harm an unborn fetus. If you’re trying to conceive, avoid going on any fad diets. Restrictive diets or eliminating whole food groups can result in poor nutritional status and malnutrition.
Women trying to become pregnant should consider preconception a time to build up a healthy foundation of nutrition to support conception and pregnancy. No one has a perfect diet (not even nutritionists). Small changes built over time have a cumulative effect.
Some ways to adopt health-promoting dietary habits include:
- Choosing whole grains over refined grains
- Eating more fruits and vegetables at meals and snacks
- Sauteing food in olive or avocado oil versus seed oils or saturated fat oils (from animals, coconut, and palm oil)
- Choose seafood low in mercury like salmon and shrimp or vegetarian sources of protein like beans and legumes
- Try to limit red and processed meats and foods as much as possible.
These food choices help to provide essential nutrients the body needs, including natural antioxidants like vitamin C and vitamin E, as well as folate, which is essential to fetal development, magnesium, iron, zinc, and B-vitamins involved in thousands of chemical reactions that occur in the body everyday. A dietitian can help to create a customized food and supplement plan that fits into your individual preferences and lifestyle.
Are you looking for customized guidance and support for your fertility journey? Contact us here!
Medical Disclaimer:
The information provided on this blog is for educational and informational purposes only and is not intended as a substitute for medical advice, diagnosis, or treatment. Always consult with a qualified healthcare provider, such as your physician, pediatrician, or a registered dietitian, before making any changes to your or your child’s diet, health routine, or treatment plan.
While we are a medical practice specializing in integrative and functional nutrition, the content shared here reflects general knowledge and holistic guidance, and may not be appropriate for every individual. Reliance on any information provided on this site is solely at your own risk.

Resources
1. Centers for Disease Control and Prevention. Infertility. Centers for Disease Control and Prevention. Published 2019. https://www.cdc.gov/reproductivehealth/infertility/index.htm
2. England CN. Female Fertility | Women & Infants Fertility Center. fertility.womenandinfants.org. https://fertility.womenandinfants.org/services/women
3. Kaufman C. Foods That Can Affect Fertility. Eatright.org. Published 2018. https://www.eatright.org/health/pregnancy/fertility-and-reproduction/fertility-foods
4. MD RHS. Fertility and diet: Is there a connection? Harvard Health Blog. Published May 31, 2018. https://www.health.harvard.edu/blog/fertility-and-diet-is-there-a-connection-2018053113949
5. Quick start to a Mediterranean diet – Harvard Health. Harvard Health. Published July 2013. Accessed August 14, 2023. https://www.health.harvard.edu/staying-healthy/quick-start-to-a-mediterranean-diet%C2%A0
6. Várbíró S, Takács I, Tűű L, Nas K, Sziva RE, Hetthéssy JR, Török M. Effects of Vitamin D on Fertility, Pregnancy and Polycystic Ovary Syndrome-A Review. Nutrients. 2022 Apr 15;14(8):1649. doi: 10.3390/nu14081649. PMID: 35458211; PMCID: PMC9029121.
7. Gupta S, Agarwal A, Banerjee J, Alvarez JG. The Role of Oxidative Stress in Spontaneous Abortion and Recurrent Pregnancy Loss: A Systematic Review. Obstetrical & Gynecological Survey. 2007;62(5):335-347. DOI: https://doi.org/10.1097/01.ogx.0000261644.89300.df
8. Unfer V, Facchinetti F, Orrù B, Giordani B, Nestler J. Myo-inositol effects in women with PCOS: a meta-analysis of randomized controlled trials. Endocrine Connections. 2017;6(8):647-658. DOI: https://doi.org/10.1530/ec-17-0243
9. Unfer V, Nestler JE, Kamenov ZA, Prapas N, Facchinetti F. Effects of Inositol(s) in Women with PCOS: A Systematic Review of Randomized Controlled Trials. International Journal of Endocrinology. 2016;2016:1-12. DOI: https://doi.org/10.1155/2016/1849162
10. Journal of Research in Medical Sciences. www.jmsjournal.net. https://www.jmsjournal.net/article.asp?issn=1735-1995
11. Kwon D, Cha HJ, Lee H, et al. Protective Effect of Glutathione against Oxidative Stress-induced Cytotoxicity in RAW 264.7 Macrophages through Activating the Nuclear Factor Erythroid 2-Related Factor-2/Heme Oxygenase-1 Pathway. Antioxidants. 2019;8(4):82. DOI: https://doi.org/10.3390/antiox8040082
12. Borcea V, Nourooz-Zadeh J, Wolff SP, et al. Alpha-lipoic acid decreases oxidative stress even in diabetic patients with poor glycemic control and albuminuria. Free Radical Biology & Medicine. 1999;26(11-12):1495-1500. DOI: https://doi.org/10.1016/s0891-5849(99)00011-8
13. Florou P, Anagnostis P, Theocharis P, Chourdakis M, Goulis DG. Does coenzyme Q10 supplementation improve fertility outcomes in women undergoing assisted reproductive technology procedures? A systematic review and meta-analysis of randomized-controlled trials. Journal of Assisted Reproduction and Genetics. Published online August 7, 2020. DOI: https://doi.org/10.1007/s10815-020-01906-3
14. James JE. Maternal caffeine consumption and pregnancy outcomes: a narrative review with implications for advice to mothers and mothers-to-be. BMJ Evidence-Based Medicine. Published online August 25, 2020:bmjebm-2020-111432. DOI: https://doi.org/10.1136/bmjebm-2020-111432
15. Adeoye O, Olawumi J, Opeyemi A, Christiania O. Review on the role of glutathione on oxidative stress and infertility. JBRA Assisted Reproduction. Published online 2017. DOI: https://doi.org/10.5935/1518-0557.20180003
16. Relative Energy Deficiency in Sport (RED-S) | Health Promotion | Brown University. www.brown.edu. https://www.brown.edu/campus-life/health/services/promotion/nutrition-eating-concerns-sports-nutrition/relative-energy-deficiency-sport-red-s
17. Hong Y, Wu S, Wei G. Adverse effects of microplastics and nanoplastics on the reproductive system: A comprehensive review of fertility and potential harmful interactions.
Science of The Total Environment. 2023; 903. https://doi.org/10.1016/j.scitotenv.2023.166258


